CUSTOMER SPOTLIGHT
DR. BRYAN GREENHOUSE, MD

Bryan Greenhouse, MD
Professor, Medicine
School of Medicine, UCSF

The Old Fight is New: Tackling Malaria with Next-Generation Sequencing
The modular targeted panel from UCSF empowers researchers across the world to take a deep-dive into the genome of P. falciparum
Malaria, a parasitic disease transmitted primarily through the bite of infected mosquitoes, is a major health threat, especially in tropical areas. It causes flu-like symptoms but can be deadly if untreated, and with 241 million cases annually, mostly in Africa, it’s a significant global concern. Recent CDC alerts noted the first US cases since 2003, but the impact of malaria extends beyond individual health – it exerts a significant economic burden on individuals, families, communities, and nations. The costs associated with malaria treatment and eradication efforts are substantial, encompassing both direct healthcare expenses and indirect costs. Conservative estimates place the direct costs at a minimum of $12 billion per year, with considerable implications for economic growth and development.
However, advances in sequencing technology have greatly boosted malaria research in recent years. Dr. Bryan Greenhouse’s team at UCSF, funded by organizations like the Bill and Melinda Gates Foundation and the National Institute of Health, leads the charge in genetics, transmission, and drug resistance studies, and they advocate for molecular surveillance to adapt to evolving challenges.
Dr. Greenhouse’s collaboration with Paragon Genomics produced a modular panel to decode parasite genomes from blood drops on filter paper, facilitating large-scale epidemiological studies. Their efforts promise to revolutionize malaria research and surveillance globally. Their tireless efforts to take this technology forward and help investigators build the genomic surveillance infrastructure in malaria-endemic countries for this disease have great potential for transforming the landscape of malaria research.
To find out more, Paragon Genomics spoke with Dr. Greenhouse in the customer interview ahead.

Can you tell us about your background? How did you get interested in the topic of malaria?
Bryan Greenhouse (BG): I had always been fascinated by the use of genomics in studying the epidemiology in infectious disease. When I was interviewing for medical residency, I read a poster from Peter Small on the micro-epidemiology of tuberculosis. At that time, I was trying to decide between a career in laboratory or epidemiologic research for infectious disease. I was interested in how these modern technological tools could be leveraged to answer the questions of disease transmission. Over the course of my career, it’s been amazing to see how much the technology has grown (both laboratory technology and the analytical capabilities) and how those two relate. In the last five years, I think we’ve reached a tipping point where the bottleneck is no longer computational tools and chemistry, but in the amount of effort we put in to develop working systems. Our lab, working closely with numerous wonderful collaborators, is thinking about how to implement and build out a system to perform surveillance more routinely, think more broadly, and answer questions about transmission in a scalable fashion.
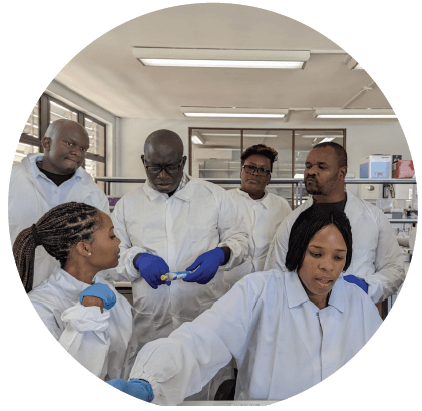
Dr. Hazel Gwarinda (Postdoc, National Institute for Communicable Diseases South Africa, bottom right) conducts malaria genomics training for the Translational Malaria Genomics (TraMGen) Fellows as part of the GenE8 projects (Genomics of Malaria in the E8).

In your opinion, what is a major challenge in genetically characterizing malaria parasites and how does your research address this?
BG: The main issue we faced was the tradeoff between throughput, number of targets, and sensitivity. Sensitivity is particularly challenging because of the sample quantity. We start with a spot of blood on filter paper so there’s not a lot of material in general, and most of the genetic material is from the human host. To compound the issue, there are often multiple strains of the parasite in a single infection and if you miss some of them, you’re not necessarily getting the right answer. There are layers of complexity- the parasite DNA is the minority of the genetic material, we want to capture the variants of the pathogen DNA, and we’re attempting to answer multiple questions about drug resistance, diagnostic resistance (evading rapid diagnostic tests via a gene deletion), and transmission epidemiology. Our team was looking for an efficient and comprehensive solution to optimize on time and cost but not compromise on the quality of the data. We spent a couple of years researching and testing different technologies, but we couldn’t find one that worked for both sensitivity and throughput until we met Paragon Genomics. After we kicked off a pilot project with Paragon, we were very impressed with the quality of the preliminary results. Once we established proof of principle and saw we could consistently generate quality data with challenging samples, our team wanted to expand the panel, scale up and apply this method at different sites globally. Customization was a key highlight. We went through many iterations of design, and the Paragon team was very open to working with us and able to get us what we needed in terms of a comprehensive and modular panel. The result is that now we have a method that does exactly what we need. And it is robust enough that the panel meets the needs of other labs and other countries.

What questions are you looking to answer and what are the goals of this program?
BG: We’re mainly looking at drug resistance, diagnostic resistance, and transmission epidemiology. An important research focus recently has been on developing new tools to better measure various aspects of transmission, including overall transmission intensity and more detailed questions such as whether malaria cases are locally transmitted or imported. This aligns well with our broader mission at the Experimental and Population-based Pathogen Investigation Center (EPPIcenter) at UCSF to perform high-quality research and answer questions relevant for public health. Equally as important is our mission to train the next generation of scientists. We focus on that locally and globally in our work with international partners. Right now, we have three collaborative projects with training components active in Africa- one across six countries in Southern Africa, another in Mozambique, and a third in Uganda.

Maria Florinda Victor Joao, a technical officer in the Angolan National Malaria Control Programme participates in a practical malaria genomics training at the National Institutes for Communicable Diseases in Johannesburg in March 2023.

Are there limitations of current gold standards or other methods, and how did Paragon Genomics’ custom targeted sequencing approach help with that?
BG: The primary limitation of other methods we have evaluated is sensitivity- we’ve tried FLASH (CRISPR-based method), which worked to some extent. However, the design process was difficult, sensitivity was limited, and the chemistry wasn’t robust- it was difficult for us to understand why certain targets were working better than others. Our lab also tried using molecular inversion probes, which had UMIs and allowed for overlapping segments in the same tube, without worrying about primer dimers. Similar to Paragon’s chemistry, it allowed us to design for many targets, but the main limitation was sensitivity. There was essentially only a single cycle for capture, compared to the 10-15 cycles for multiplex PCR (mPCR). In the past, when I was working with microsatellites, I developed my own homebrew mPCR and designed my own primers, but it was difficult to expand the number of targets. And because we had such a robust solution out-of-the-box with Paragon, it was much more efficient for us to continue with a proven strategy.

Dr. Jessica Briggs leads the Malaria Genomics and Data Analytics Workshop in Kampala, Uganda in September 2022.

How did you approach the panel design process? How did you develop the modular approach and what advantages does it offer?
BG: Andres Aranda-Diaz (Assistant Researcher) was the one who initially proposed a modular approach with different primer pools based on the application (drug and diagnostic resistance or transmission and population genetics) – he asked, why waste your sequencing reads on a question you’re not interested in answering? But we also wanted to maintain the flexibility to pool primers together if we did want to investigate multiple questions simultaneously.
So we developed these modular primer pools that would allow us to customize by use case- we can use one pool for each and require fewer reads or combine two together and investigate a larger number of targets. We ended up developing several sizes for the drug resistance primer pools as well, one which is smaller and more sensitive but covers the most important targets, and a larger one which contains additional experimental targets for research purposes. We’ll continue to refine the primer pools and informatic tools, pending new content we’d like to add, but this is a great starting tool for understanding population genetics, transmission dynamics, etc.

What do you see as the biggest advantages of using a custom targeted NGS panel for malaria research or diagnosis, and how does your panel maximize those benefits?
BG: The biggest advantage is probably the reliability of the workflow. Maybe there are other methods out there that are as simple but there’s something to be noted about the consistent data quality from Paragon’s chemistry. We haven’t needed to repeat many experiments or throw out data from many samples, which happened more frequently with the other methods we tried. The high uniformity of balance between targets and samples and high sensitivity have been big advantages. We’re working on automation right now, and hope that it will make processing a large number of samples even easier.

How is the data looking? Are there any exciting discoveries you can share with us?
BG: I’d love to refer people to a pre-print that we released based on a colleague’s study in Ethiopia. The Horn of Africa is currently experiencing a triple-threat for malaria: drug and diagnostic resistant parasites being spread by an invasive mosquito, Anopheles stephensii. Our collaborators saw a surge in malaria cases and wanted to understand what precipitated such an outbreak and if there were any concerning mutations in the spreading parasites. Our collaborators sent samples from the field to our lab because we had this modular panel that could answer many questions in parallel. We were able to uncover with the sequencing data that the outbreak originated from just a few genetically distinct parasites that appeared to spread like wildfire by Anopheles stephensii. Data from the diversity module of the panel demonstrated that the outbreak essentially consisted of two clones. We discovered one of these clones had gene deletions associated with diagnostic resistance, consistent with these infections being missed by rapid diagnostic tests, and drug resistance for one of the most important classes of malaria medications (artemisinins). The multipurpose targeted NGS panel we developed with Paragon enabled us to efficiently determine these details about the epidemiology and drug resistance all at once.

How do you see NGS panels evolving in the field of malaria research and clinical practice and how do you think your panel will contribute to that evolution?
BG: We want to continue to have easy and small panels for existing applications. We’ve also been thinking about something called therapeutic efficacy studies- when we evaluate if a malaria drug works, we treat patients and then follow them for many weeks. But if a patient comes back a few weeks later with a reinfection, you need to know if the infection is the original infection (indicating they failed therapy) or if it’s an entirely new infection, indicating the drug worked well and the patient happened to get infected again. We need to identify if the parasites are the same or different. It’s been difficult because of the cumbersome methods in the past, but amplicon sequencing would be very useful in this application, particularly given the high sensitivity to detect most of the parasites present and the ability to simultaneously evaluate a number of diverse targets. As we think about leveraging the current panel and tailoring it for specific therapeutic efficacy studies, we want to statistically curate a subset of the panel (e.g. ~20 targets) for the most efficient sequencing. Our team has also been thinking about investigating interesting biological questions like how immunity develops. We want to sequence those malaria targets of the human immune system where genetic variation exists and examine associations with infection outcomes in our cohort studies and the associated immune response.

What’s next for your team? Are there any plans to improve or expand the panel? How do you anticipate the technology to evolve in the coming years?
BG: We see a lot of potential with long-read technology, especially as it gets more accurate and less expensive. I think it’s particularly relevant in some African sites since the sequencer is so portable and affordable- there’s no need for large capital equipment. We are also really interested to study regions and genes relevant to immunity, but they are frequently longer than the 300-600 bases which can be read with current short-read sequencing. Of particular interest are var genes in malaria (variant surface antigens), which can be a few thousand bases long and difficult to assemble with short-read sequencing as there’s a lot of diversity and mitotic recombination. I foresee us continuing to evolve panels, learning from our experience and developing panels for specific use cases and specific users, instead of a one-size-fits-all approach.

Could you share any anecdotes or stories that illustrate the impact of your research?
BG: The trainees are super excited! We first talked about the technology conceptually, specifically why we opted for NGS instead of qPCR. As they’ve gotten hands-on training, and have generated good libraries themselves, it’s empowered them. They see how simple the workflow is, and as they generate the data, they see it’s within their reach.
This latest training in South Africa and seeing the team be able to get everything up and running in two weeks in Gambia has been so rewarding. The more routine this type of work becomes, the more we can work as a community, and build tools to share the results. Ultimately we’d like to build towards contributing data to regional or global repositories like we have for COVID-19, a resource which has been so valuable.
Our team has started a monthly online seminar series with all current users (National Institute for Communicable Diseases South Africa, Infectious Diseases Research Collaboration Uganda, Centro de InvestigaC’C#o em SaC:de de ManhiC’a, MoC’ambique, Instituto de Salud Global Spain, Medical Research Council Unit The Gambia, National TsingHua University Taiwan, Yale University USA) to create community and enhance collaborations. And we’re actively working on finding other ways to have forums where they can discuss results, roadblocks and ideas, and troubleshoot together.

Dr. Blazenka Letinic (Postdoc, NICD, center left) conducts malaria genomics training for the Translational Malaria Genomics (TraMGen) Fellows. Picture shows TraMGen Fellows from different regions in Africa.
References
- Nature Communications: Genomic malaria surveillance of antenatal care users detects reduced transmission following elimination interventions in Mozambique
- Centers for Disease Control and Prevention. (n.d.). Malaria worldwide: Impact of malaria. https://www.cdc.gov/malaria/php/impact/
- Center for Disease and Control. June 26, 2023. Locally acquired malaria cases identified in the US. https://emergency.cdc.gov/han/2023/han00494.asp
Acknowledgements:
- Bioinformatics: Nick Hathaway, Max Murphy, Inna Gerlovina, Brian Palmer
- Andrés Aranda-Díaz, UCSF Assistant Researcher
- Jessica Briggs, UCSF Assistant Professor, P.I. for IMMRSE-U: Implementing Malaria Molecular Surveillance in Uganda.
- Jennifer Smith, UCSF Associate Professor and Senior Research Scientist at the Malaria Elimination Initiative (MEI), P.I. of GenE8: Genomics of Malaria in the E8, in collaboration with the Elimination Eight Initiative (E8).
- Collaborators in Africa: Jaishree Raman (NICD South Africa), Issac Ssewanyana (IDRC, Uganda), Alfredo Mayor (ISGlobal, Spain, and CISM, Mozambique)